Assessing Functional Asymmetries After Injury
Part 1: the Journey Continues
I struggled early in my career to marry science with coaching. I lived in a dichotomy. I was a graduate student completing a Master of Science in muscle physiology, doing all kinds of neuromuscular testing. I would then leave the lab and head down to the weight room to coach athletes. I found it hard to bring science into the weight room in a meaningful way. The testing methods I was using were either (a) noisy (b) impractical or (c) not sensitive to performance or reducing the impact of injuries.
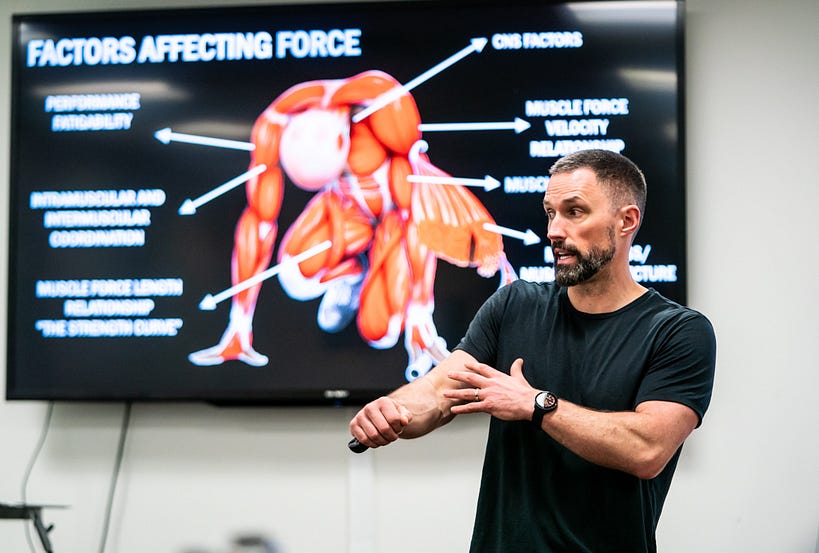
Photo Dave Holland, Canadian Sport Institute Calgary
The problem was two-fold. First, I lacked the right question. Second, I lacked the right equipment. I lucked out on both fronts after attending a conference in Colorado Springs where I met Per Aagaard, who would eventually become my PhD supervisor and Bill Sands, who pointed me to an affordable force plate system made by a company called Pasco. Cost had always been the barrier for me acquiring force plates. Consequently, I spent a lot of time (and money) on subpar systems that weren’t helping me. We purchased the Pasco system but needed two force plates to do our testing as they were quite small.

Pasco portable force plates. Image from performbetter.co.uk
After they arrived, I quickly found out that not only could I use the force plates to assess strength and power abilities but also, I could track lower limb asymmetries by comparing the force-time curves from the right and left sides. With respect to the former, I learned that vertical jump force-time analysis was no joke for a muscle physiologist with a relatively limited background in computer coding. I found myself hand-bombing vertical jump force-time curves, and tediously performing force-time integration calculations to get at the metrics of interest. Much of my thinking on force-time analysis was shaped by Per Aagaard. I was amazed that I could pull nearly 100 outcome measures from a vertical jump (but I admit, only 10–20 were useful).
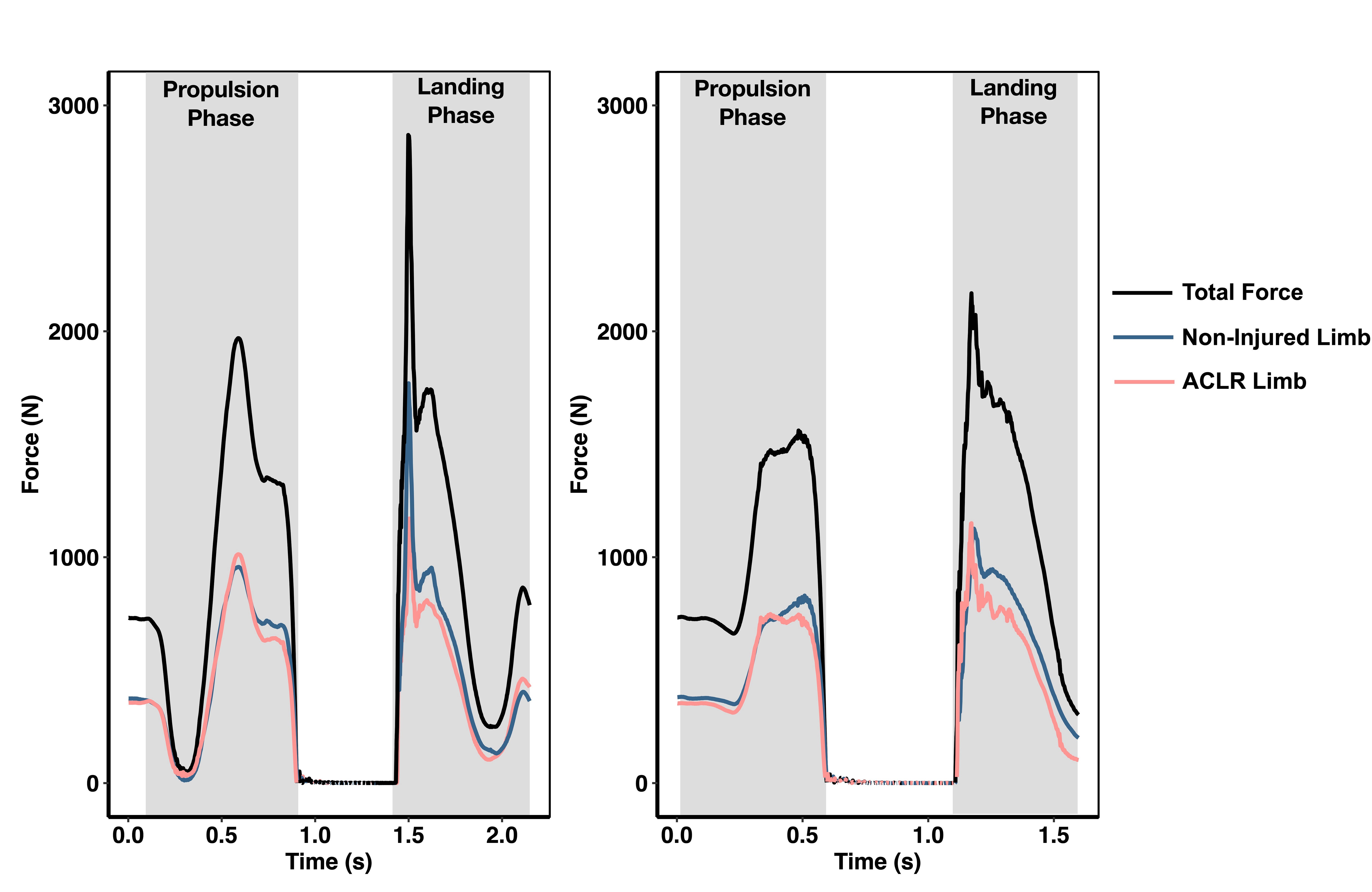
Force-time curves from the Pasco force plates.
However, with respect to the latter (i.e. measuring lower limb asymmetries), I found immediate value by just looking at the force-time curves themselves. I didn’t have to do any analysis to see that the right and left lower limb force-time curves reflected neuromuscular deficits I couldn’t see with my eyes in the injured athletes I was working with. And importantly, the force-time curves were sensitive to the recovery process after injury. This meant that I could track athletes as they were recovering from lower body injuries (and lumbar spine injuries), improving my ability to contribute to return to health, return to sport, and return to performance discussions with my colleagues. After years of feeling like I was living in a dichotomy, I was finally merging science with practice in a meaningful way.
Why it Matters
Injuries are inherent in elite sport. Some injuries are worse than others. And some injuries are life altering. After an injury, an athlete usually relies on a team of experts to support the return to health, return to sport, and return to performance transition. I emphasize the words return to health, sport, performance, and transition. Problematically, many sport science/sport medicine practitioners see only return to sport and instead of a transition, return to sport testing is treated more like a final exam. If an athlete passes, we give them a high-five and they’re back to sport. Oftentimes, they never perform another test again related to their injury. If they fail, they’re held off the field to let a bit more time pass.
However, we know that deficits arising from lower body injuries like anterior cruciate ligament (ACL) tears can last for years. Further, athletes are at highest risk for reinjury in the two-year period after the primary injury was sustained. So, how does testing at 9-months after an ACL reconstruction surgery (ACLR) predict an injury that might happen more than a year later? It probably doesn’t.
It’s interesting that many of us rely solely on time from injury as the primary determinant of return to sport readiness but many of us know this is highly inadequate. Time from surgery has little bearing on neuromuscular function. Neuromuscular function is highly dynamic and complex and affected by all sorts of factors like fatigue and psychology. Nevertheless, we often treat return to sport readiness in the sterile environment of a laboratory and in a highly static manner. We assume that a single testing time point tells us all we will ever need to know about a potential risk for reinjury.
Image from pixabay.com
As I was working daily with a dual force plate system to assess lower limb asymmetries, I realized that our professional community needed better testing methodologies to evaluate athletes after injuries were sustained. This spurred my PhD research. The accepted standard at the time was functional performance testing, like a single or triple leg hop for distance.
But athletes are master compensators and they often achieve performance benchmarks while masking deficits. Vertical jump force-time asymmetry testing opened up a new set of metrics and insights surrounding the functional capacities of the injured athletes I was training. They had a much harder time disguising their compensation strategies when I could visualize how they were applying force into the ground. I was using a valid and reliable test protocol that was sensitive to the time-course of recovery after injury to enhance my coaching eye.
I’ve written and spoken about the importance of recording simple metrics consistently over time to build a pre-injury baseline against which we can compare an injured athlete throughout the post-injury period. Tracking how neuromuscular function is changing before and after an injury is the starting point for understanding why things are changing and how to make it better.

Photo Dave Holland, Canadian Sport Institute Calgary
Interlimb asymmetry testing with a dual force plate system is a practical solution for building a functional baseline on athletes. With the commercialization of analytical software, practitioners can extract important information quickly and efficiently. Owing to the persistent strength and power deficits incurred after lower body injury, interlimb asymmetries paint a functional picture that can guide decision making.
We can dig under the hood to determine how an injured athlete achieved a performance benchmark. We can identify trainable deficits that can’t be seen with our coaching eye alone that can bolster resilience against reinjuries. Measuring what matters, matters most when athlete health and safety are on the line.
