Musculoskeletal Telehealth
Thoughts from a Physiatrist in Virtual Practice during COVID-19
Overview: A case example using video and a wearable insole sensor to assess individuals with musculoskeletal complaints.
Telehealth Clinic
For the last few weeks I’ve been assessing individuals exclusively via telephone or video due to COVID-19 precautions. There are some clear benefits to a Telehealth practice: patients don’t need to travel or pay for parking and I can easily show web-based resources with a screen share.
Studies have shown that for chronic musculoskeletal complaints and concussion there is a high level of agreement between in-person and Telehealth assessments and patient satisfaction is high (1–3).
The biggest drawback is obvious: I can’t examine individuals with my hands! As a musculoskeletal medicine physician I feel like my stethoscope has been taken away because I can’t palpate painful structures.
As a result I’ve been relying heavily on technology. Inspection of walking, a squat and single leg hops via video is something I’ve implemented in all new consults. I ask patients to ensure they have enough space nearby to ambulate, squat and jump. At times I’ve asked them to recruit a family member to hold their mobile device or computer to get a better view. To do this, I use an EMR with a built-in video platform. Patients are sent a link prior to their appointment and can sign on with their mobile phone or computer.
Case Example: Chronic low back pain
History
A 36 year-old male with a history of chronic episodic left-sided low back and buttock pain. This began after a car accident over 10 years ago where he wasn’t injured too badly, he just hasn’t felt quite right since. He has no red flags on history. No radiating pain, no weakness distally in the foot, no numbness or tingling, no morning stiffness, and no night pain. He has been weight stable and has normal bowel, bladder and sexual function. Otherwise well, taking no medications.

Mechanical Low Back Pain
He describes his episodes of low back pain as acute onset, usually after prolonged sitting or large increases in training volume. The pain has a catching sensation which localizes to the left buttocks and can sometimes radiate to the left thigh (above the knee). No change with sitting or standing. Worse bending forward and raising to stand. Laying down relieves his pain somewhat. So does heat. After 2–3 days of reduced activity symptoms generally return to baseline.
He has become quite frustrated with this pattern of dysfunction and is wondering what, if anything, he can do to limit his day-to-day symptoms.
He has not had any imaging.
Video Exam
Well appearing male of stated age. Not in distress. When asked to “point with one finger” to the region of greatest discomfort, he points to his left sacroiliac joint.
Gait is symmetric. Normal head and trunk posture. Normal arm swing. Step width within normal limits. Heel to toe progression within normal limits. Symmetric right to left step lengths. Normal ankle-knee-hip movements with perhaps some mild out-toeing of the left foot relative to the right. Heel and toe walking are normal. Repeated heel raise did not reveal any weakness.
In a deep squat he off-loads the left hip and most weight acceptance is on the right. During jump testing his left leg shifts into valgus at the knee during landing (the eccentric deceleration phase of jumping).
No pain in the FABER position and negative straight leg raise. No pain with abduction of the thigh when laying in the lateral decubitus position.
Clinical Impression
A 36 year-old male with mechanical low back and buttock pain that localizes to his the region of the left sacroiliac joint. I suspect functional left gluteus medius weakness based on the physical exam findings of out toeing on the left and valgus shift at the knee during jumping and squatting. The gluteus medius muscle is largely responsible for hip abduction in standing and when weak, medial collapse of the distal femur creating valgus alignment at the knee results.
The differential diagnosis for gluteus medius weakness in the context of chronic episodic mechanical low back pain includes:
Chronic L5 radiculopathy
L5-S1 facetogenic pain
Sacroiliac joint irritation
Atrophy of the gluteal muscles due to pain inhibition from the above
Reciprocal inhibition of gluteus muscles from tight hip flexors
The episodic nature of his pain history combined with his age, a positive Fortin finger sign and an absence of prolonged morning stiffness has me leaning toward sacroiliac joint pain secondary to pelvic dysfunction as the diagnosis. Gluteus medius weakness is likely due to pain inhibition.
He has no red flags on history suggestive of an autoimmune pathology like ankylosing spondylitis. With no pain or numbness past the knee and no weakness to plantar or ankle dorsiflexion I am less likely to order advanced imaging (e.g. MRI of the lumbar spine) or electrodiagnostic studies to investigate lumbar disc herniation or radiculopathy. Non-inflammatory sacroiliac pain and pelvic ring dysfunction falls into the controversial category of “mechanical low back pain”.
Other Remote Physical Examination Tools
I’ve been wondering how a remote monitoring device like Plantiga, a wearable insole sensor that collects data on walk/run and jump activities, could augment video assessments in a Telehealth setting. Wearable sensors are on the rise in orthopaedic rehabilitation and monitoring athletic performance and assisting in determining readiness to return to sport (4).
This individual has his own personal Plantiga system so he shared his data with me for review.
Plantiga Walk Test
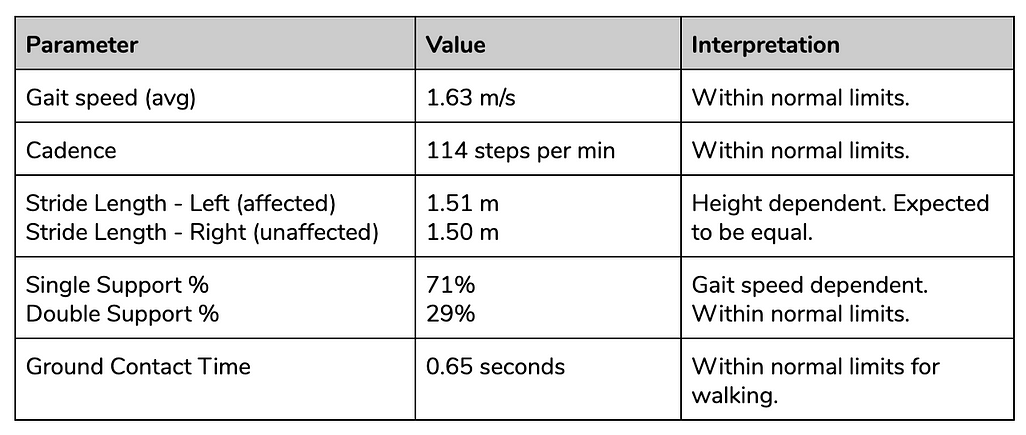
Plantiga Walk Test Data
From the walk test gait parameters I can see that this individual is a healthy male in his 30’s ambulating at a speed within normal limits for his age. He does not appear to have a pathological gait. Stride length is within normal limits for his height.
In addition to gait parameters Plantiga measures g-Force, which is an outcome measure I’m somewhat unfamiliar with. Essentially the insole sensor houses an inertial measurement unit (an IMU) which captures accelerations from each foot as it moves through the gait or jump cycle. From this we can determine the intensity of impact (g-Force per minute) during a walk test.
Plantiga Walk Test g-Force
Plantiga Walk Test g-Force
Over the course of a 2-hour open activity, the cumulative load on the left limb was 40k g-Force and the cumulative load on the right limb was 36k g-Force. These results indicate higher accelerations of the left foot. I suspect we’re capturing the out-toeing of the left limb seen from his video assessment but this may also represent a loss of hip extensor eccentric control during terminal swing to heel contact.
Plantiga Jump Tests
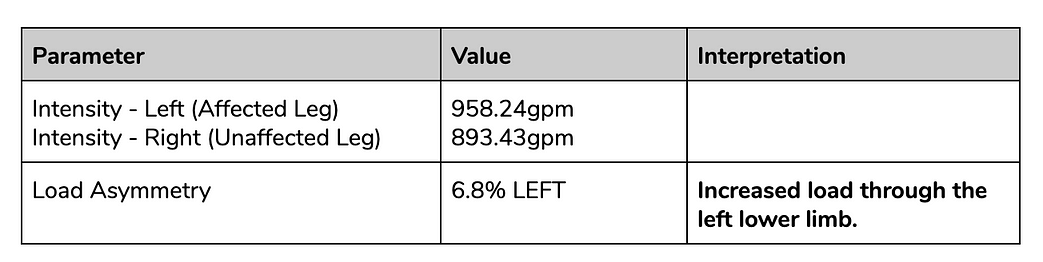
Plantiga Jump Test Data
From the jump tests I can see that this individual has good athleticism as indicated by his relatively high reactive strength index (RSI). In Dr. Matt Jordan’s post on RSI he suggested multiplying the modified RSI output Plantiga gives by 3. A score greater than 2.5 is good and a score lower than 1.5 was considered poor and the athlete is not ready to return to sport.
Looking at the results of single leg jump for height and distance, he is weaker on the left more so in the vertical jump as compared to horizontal jump. This indicates that his ankle complex and plantar flexion power is largely intact. In vertical jump, approximately 40% of propulsive force is coming from the hip extensors, 20% from the knee extensors and 40% from plantar flexors (5).
Additional Conclusions Using Plantiga
Normal objective gait parameters.
Confirms video inspection findings of hip extensor (gluteus medius) weakness and quantifies the limb asymmetry using jump tests.
Demonstrates that functional ankle plantar flexor power (L5-S1 innervated muscles) is reassuringly intact.
Provides a baseline measure to gauge response to treatment.
The clinical utility of wearable technology in a busy musculoskeletal medical practice is an important research question that needs further investigation.
Next Steps
The results of my history, physical examination by video and the wearable insole sensor walk and jump tests are reassuring. His left gluteus muscle weakness is most likely functional and certainly SI joint irritation or pelvic ring dysfunction may be contributing. He does not need advanced imaging or electrodiagnostic studies at this time.
First line treatment for this individual with mechanical low back and buttock pain is exercise therapy and in particular, gluteus medius strengthening.
Recommended exercises include:
Side plank
Side box step-ups
Split squats
One-leg lunges
Lateral band walks
Banded squats with side leg lifts
Skater jumps
Once COVID-19 precautions are lifted and non-essential medical services can resume with proper personal protective equipment this patient requires a complete physical examination. In my view, Telehealth + Technology doesn’t replace the in-person exam. But for now I’m confident in prescribing him strengthening exercises and scheduling a follow-up for a later date.
Should his pain and lower limb asymmetry on jump testing persist despite an appropriate strengthening program over the next 3–4 months I would then consider further advanced imaging or sequential injections to delineate the pain generator and treat it.
Limitations to musculoskeletal assessment using Telehealth
Telehealth itself does not have a standardized definition in the literature, and the use of this technology varies between providers and patient populations; determining clinical outcomes compared with in‐person traditional visits is challenging to quantify — Tenforde et al. 2018
Telehealth Musculoskeletal Assessment Tips
Ensure patients understand Telehealth assessments will include a visual and functional inspection via video.
Gait, squat and jump tests are essential Telehealth functional movement tests for musculoskeletal physicians.
Consider adding an objective measurement tool which can assist in quantifying limb asymmetries and assist in tracking individual responses to interventions like strength training or injections.
Schedule a follow-up for an abbreviated history and complete physical exam when appropriate.
Guest Author - Dr. Kaila Holtz is a Physiatrist based in Vancouver, Canada. She specializes in musculoskeletal pain, osteoarthritis management, overuse sports or occupational injuries (e.g. running, pitching, sitting). She is the Medical Director of Triumph Health and Chief Medical Officer at Plantiga. When not in the clinic she is chasing her toddler and training for a half-marathon. Find her on Twitter @kailaholtz.
References:
B.B. Vargas, D.D. Channer, D.W. Dodick, B.M. Demaerschalk. Teleconcussion: An innovative approach to screening, diagnosis, and management of mild traumatic brain injury. Telemed J E Health. 2012; 18: 803–806.
Tenforde, A.S., Hefner, J.E., Kodish‐Wachs, J.E., Iaccarino, M.A. and Paganoni, S. (2017), Telehealth in Physical Medicine and Rehabilitation: A Narrative Review. PM&R, 9: S51-S58.
Cottrell, M. A., O’Leary, S. P., Swete-Kelly, P., Elwell, B., Hess, S., Litchfield, M.-A., McLoughlin, I., Tweedy, R., Raymer, M., Hill, A. J., & Russell, T. G. (2018). Agreement between telehealth and in-person assessment of patients with chronic musculoskeletal conditions presenting to an advanced-practice physiotherapy screening clinic. Musculoskeletal Science and Practice, 38, 99–105.
O’reilly, M., Caulfield, B., Ward, T., Johnston, • William, & Doherty, C. (2018). Wearable Inertial Sensor Systems for Lower Limb Exercise Detection and Evaluation: A Systematic Review. Sports Medicine, 48, 1221–1246.
Robertson, DG., Fleming, D., Kinetics of standing broad and vertical jumping. Can J Sport Sci. 1987 Mar;12(1):19–23
This content is for information and educational purposes. It is not intended to substitute for the advice of a physician. You should always consult your doctor for specific information on personal health matters, or other relevant professionals to ensure that your own circumstances are considered.

